The numbers, labels and descriptions pertaining to medical patients and COVID-19 cases that are housed in electronic health records may seem to be nothing more than a track record — a jumble of information a physician updates, typing away as their patient sits down for a visit. But to public health researchers, data from public health documents, when analyzed, can tell a story — a story with a moral.
Two University projects involving collaboration with other state organizations are in the works, binding together pages of health information in an effort to learn from the pandemic and improve health care.
Bioinformaticians form “A Learning Health Care System in Rhode Island for COVID-19”
Researchers at the University and the Rhode Island Quality Institute have partnered to analyze vast amounts of medical data to identify trends in an attempt to improve health care in the state and the nation. They’ve dubbed their effort “A Learning Health Care System in Rhode Island for COVID-19.”
As the pandemic has progressed, medical professionals have been interested in the ways in which someone’s medical history and demographics factor into their susceptibility to COVID-19 and its symptoms. But still, there is much to be understood.
To make appropriate decisions, health care providers may refer to prior medical data in order to predict which patients (based on their medical histories) will likely need to receive more critical treatment sooner in the event of another wave of COVID-19 or similar infectious diseases.
“Going forward, we would want to understand what impact underlying conditions may have on an individual and maybe even guide treatment,” said President and CEO of the Rhode Island Quality Institute, Director of the Center for Biomedical Informatics, Associate Professor of Medical Science and Associate Professor of Health Services, Policy and Practice Neil Sarkar, a co-principal investigator of the study.
More broadly, interpreting this data through informatics research can help improve health care in general, and data following the implementation of these changes can indicate whether those changes were successful. And so the cycle continues within the learning health care system, said Elizabeth Chen, interim director of the Center for Biomedical Informatics, associate professor of medical science and associate professor of health services, policy and practice and co-principal investigator.
The data collected may also correlate COVID-19 testing with geographic areas based on patients’ access to resources and, in putting “a magnifying glass” on inadequate living conditions, could reveal which communities need further support, Sarkar said.
“Health disparities in particular, health equity is a real challenge for us,” he said. “And they’re pretty stark here in Rhode Island.”
The clinical information for this University and state project includes Rhode Island COVID-19 test results coupled with each patient’s medical history available through CurrentCare — the state’s platform through which health information that patients have consented to share may be exchanged between groups for research purposes, Sarkar said.
To ensure privacy and confidentiality, the researchers have separated the data from any direct identifying information and are strengthening infrastructure to securely hold it. These efforts are part of the Brown Center for Biomedical Informatics’ Unified Research Data Sharing and Analysis Initiative and involve collaborations with other University and Rhode Island organizations, Chen said.
From “structured” data, like patient demographics, medical measurements, diagnoses, performed procedures and prescribed medications, to “unstructured” data that comes in the form of clinical notes in the electronic health record, researchers can extract a plethora of information dating back to 2012, Chen said.
But these data often start off disorganized and vary in format, so they first have to be “cleaned,” standardized and transformed for accessibility, Chen said.
Once the data is easy to compare, statistics and machine learning algorithms can be used to detect patterns and construct models that could help researchers draw broader conclusions and make predictions about different patient populations.
These findings may then be transferred directly to health care providers through tools they already use to inform their clinical decisions.
The study’s specific data, which only includes Rhode Island, may then be integrated with findings obtained through similar research efforts across the country, Chen said. For example, the Consortium for Clinical Characterization of COVID-19 (4CE) and the National COVID Cohort Collaborative (N3C) are hoping to answer similar questions for the entire United States population. This consolidation of data will require additional work from R.I. researchers to establish the necessary infrastructure to put the data in a format that matches that of these other organizations.
Other University faculty in medicine, the social sciences, public health and computation-based departments, among others, served as co-investigators. Additional staff and students from the University and the Warren Alpert Medical School are contributing to the work, and the researchers hope to eventually bring the Rhode Island Department of Health, clinicians and patients into the conversation.
“While we’re focused on the research, the data to knowledge — really the ultimate goal is to put it into practice, … to help clinicians and public health providers help address COVID” at local, national and international levels, Chen said.
Clinicians, public health experts learn from COVID-19 data
Researchers from Rhode Island Hospital and the Department of Health have also joined forces to gather information to help predict what kinds of COVID-19 patients will require the most critical care and help hospitals decide how to distribute their resources accordingly.
“For a large part, science has ruled the day here in Rhode Island, which is nice, including through public health,” Chan said. “I think that’s why we’ve been able to flatten the curve and have a low prevalence of COVID-19 in our state.”
The data for this study comes from a record of COVID-19 related hospitalizations in Rhode Island. Counting hospitalized patients originally helped the state track the spread of the pandemic, but can also inform clinical decision-making.
The team is studying data on demographic and health factors for present and former Lifespan hospital patients. They are trying to see which factors, such as old age or health conditions like obesity, are associated with more severe COVID-19 cases in Rhode Island, which may differ from other states, said Eleftherios Mylonakis, professor of infectious diseases, professor of medicine, assistant dean of medicine and professor of molecular microbiology and immunology.
The researchers hope to apply information from a database they have compiled on hundreds of patients “to build knowledge and tools that are going to help physicians in managing these patients,” said Fadi Shehadeh, research associate in medicine and a collaborator on the project. Using artificial intelligence, these tools would make predictions about the progression of COVID-19 in individual people, such as the likelihood of death.
Once ready, the team’s simulation models will factor in relevant patient characteristics to calculate expected outcomes if infected with the virus.
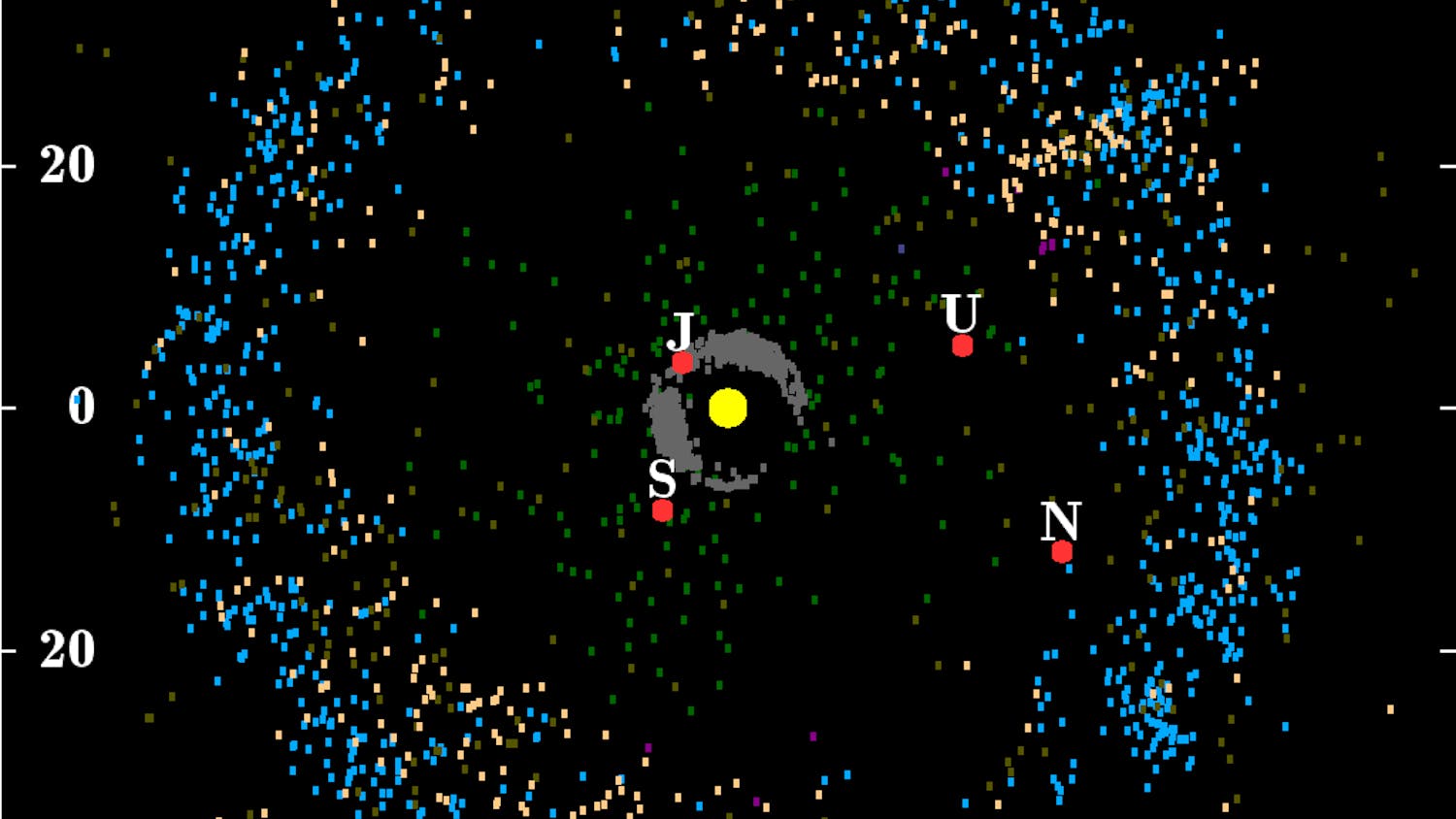
Examining the spread of COVID-19 in Rhode Island through modeling is another aspect of their project.
Beyond COVID-19, the research has strengthened the bridge connecting the state’s hospitals and RIDOH, and the investigators hope to “learn also a lot of lessons from COVID-19 that we can implement in other diseases,” Mylonakis said.
Collaboration between institutions and departments has stood out as another benefit of the COVID-19 research, Chan said. Other members of this group include Assistant Professor of Medicine Jun Tao, who previously worked at the Chinese Center for Disease Control and Protection.
The Brown COVID-19 Research Seed Fund awards have gone towards supporting “junior people who are going to develop the expertise and use the expertise to improve the lives of people in Rhode Island,” Mylonakis said.
“It’s been really exciting to see ... our state respond,” Chan said. “Rhode Island really has been at the forefront of addressing COVID-19.”
In addition to the 15 projects across departments, disciplines and organizations that received kickstart funding from the COVID-19 Research Seed Fund, University research on the pandemic has not been limited to these investigations.
But through the Seed awards, “Brown has given the appropriate signals to the community of how we’re all together on this, how science is … important in helping answer the local questions,” Mylonakis said.
In turn, “Brown researchers have shown tremendous dedication to the health and safety of the community, and to finding innovative ways to respond to the COVID-19 pandemic,” Vice President of Research and Professor of Mathematics Jill Pipher wrote in an email to The Herald.

ADVERTISEMENT