Christianson syndrome, also referred to as CS, is a rare neurodevelopmental disorder associated with seizures, various degrees of intellectual disability and difficulty standing or walking. Research suggests that cells expressing characteristics related to the condition respond differently to treatment depending on the type of underlying mutation in a gene associated with the syndrome, according to findings published in Science Translational Medicine Feb. 10.
University researchers from the Morrow lab led the study by testing two treatments, which both involved first reprogramming blood cells to neurons.
Although CS is “becoming increasingly diagnosed,” there is “little known about the neural mechanism behind the disease (and) therapeutic options for patients remain limited,” Anne McKinney, a professor in the department of Pharmacology and Therapeutics at McGill University, who was not involved with the research but has studied the syndrome, wrote in an email to The Herald.
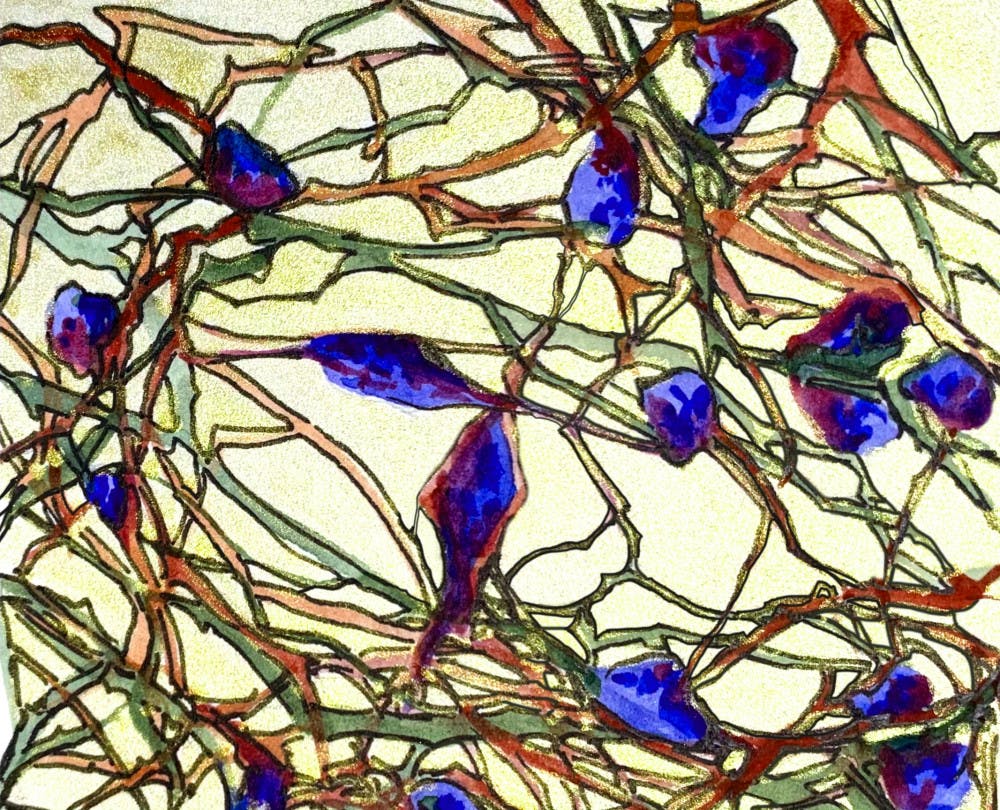
CS affects the NHE6 protein, which controls the concentration of protons in a component of cells known as the endosome. Mutations in the protein raise the concentration of protons, impacting endosome function. This change is associated with the adverse neurological effects in CS, according to Sofia Lizarraga, assistant professor in the Department of Biological Sciences at the University of South Carolina.
The condition is genetic and recessive X-linked, so a person who has all copies of their X chromosomes carrying the mutated NHE6 protein will express the disease.
“We know from our previous studies in mouse and now human neurons that NHE6 is important for the maturation of neurons … and neuronal function,” said Lizarraga, who began working on this project when she was in the Morrow lab and is one of the lead authors of the study.
Lizarraga and the rest of the researchers “wanted to develop human experimental systems where we could actually understand the NHE6 protein in humans and also test potential therapeutic strategies,” she said.
To develop these systems, the researchers collected blood samples from five male patients and their unaffected brothers as controls. The samples, which contained the red blood cells used for a later part of the experiment, were obtained from the Bradley Hospital in Rhode Island.
“Several labs use skin cells, but you can use any type of cell to reprogram them” into stem cells, Lizarraga said. “It is less painful to draw blood than to make a skin patch, which is why we used blood cells,” she explained.
The researchers first reprogrammed the blood cells into stem cells before making the neurons in order to have a population of stem cells they could freeze and refer back to if needed. “If you have stem cells, not only can you make neurons, but you can also make other types of cells in the brain, so there is a lot of potential having made the stem cells first,” Lizarraga said.
Since this approach allowed the stem cells to “retain the unique genetic signature of the individual from whom they were derived” and be further studied using the patients’ known medical history, this study is “extremely exciting,” McKinney wrote. This is a “first step on the road toward neurological personalized medicine,” she added.
Using this technology, the paper focused on five different types of CS mutations. Four of these mutations were nonsense mutations — mutations that create a truncation in the protein — and one that was a missense mutation — a mutation that substitutes one protein building block for another.
“Patient mutations fall into distinct classes that may show different responses to therapeutic strategies,” Eric Morrow, senior author of the study and associate professor of biology and psychiatry and human behavior, wrote in an email to The Herald.
The researchers tested two treatment strategies on the neurons derived from patient blood: growth factor treatment and gene transfer.
Neuronal growth factors are molecules that help neurons develop. Gene transfer is a procedure that was used in this study to insert a healthy copy of the gene encoding the NHE6 protein in cells originally lacking the correct version of the gene, according to Lizarraga.
The researchers found that all five types of mutations could be rescued using specific kinds of growth factors, while only nonsense mutations responded to the gene transfer treatment.
The “million dollar question” is why this is the case, Lizarraga said. “We think it’s because in the nonsense mutation you don’t have NHE6, you're just putting in a healthy copy of NHE6 that can replace the function that is lost.”
The missense mutation, meanwhile, is due to a mutated rather than truncated protein, so “even if you (add) more healthy protein,” the missense mutation “might be preventing the healthy copy from functioning well,” Lizarraga added.
This study’s findings may allow researchers to begin developing “potential therapeutic targets and possible gene therapies to improve the quality of life,” not only for Christianson syndrome patients, but also for individuals suffering from other disorders “where NHE6 is perturbed,” McKinney wrote.
Lizarraga said that the “main takeaway” from the experiment is that when developing “future therapeutics for Christianson syndrome, it's important to pay attention to the specific mutations that patients have because the same protein can be mutated in different ways, and the different mutations can affect how patients respond to treatment.”
Gabriella is the Senior Science & Research Editor of The Brown Daily Herald. She is a junior from San Francisco studying neuroscience on the premedical track.