Polyploidal cancer cells, also known as giant cancer cells, have been brought into the spotlight as new research suggests their previously unknown involvement in cancer development and remission.
Researchers found that normal cancer treatments led to an increase in these giant cancer cells, and this prompted research into exactly what their function was, said Michelle Dawson, assistant professor of molecular pharmacology, physiology and biotechnology.
Other people have looked at polyploidal cells before, but most clinicians had viewed them as “dead-end cells” as they do not undergo mitosis, Dawson said.
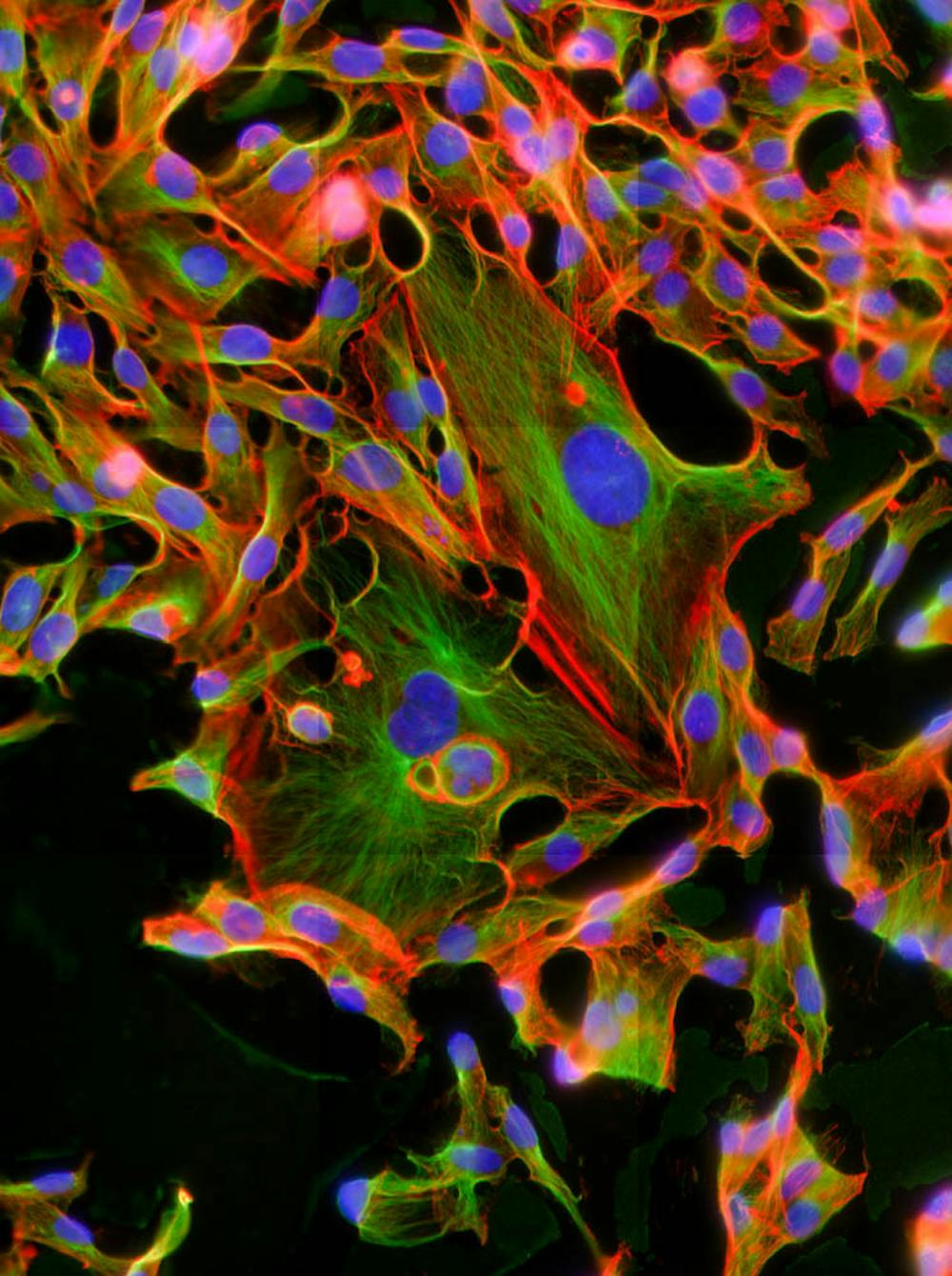
A polyploidal cancer cell, which is 10 times the size of a normal cancer cell, has multiple chromosomal copies, Dawson said. The giant cell undergoes amitotic budding, when it splits and produces a “normal” cancer cell with an abnormal number of chromosomes. So, if there are more giant cells, this can cause cancer cells to proliferate, she added.
“These cells are present in more aggressive types of cancer tumors,” said Deepraj Ghosh, postdoctoral research associate in Dawson’s lab. “They have been more resistant to chemotherapy drugs and act like a cancer stem cell, giving rise to a higher population of cancer cells, making them harder to treat,” he added.
“It turns out that within a cancer cell population there are 1 to 2 percent of these giant polyploidal cells that exist,” Dawson said. If cancer is treated with common chemotherapy, such as Taxol or radiation, the number of giant cancer cells increases to between 20 and 90 percent, she added.
“We have looked at breast and ovarian cancer, and the amount of polyploidal cells varies initially, but treatment is what gives rise to five to 10 times more of these cells,” said Botai Xuan, a PhD candidate in the lab.
Another problem is that there are so many cells in tissues that the likelihood of finding the 1 percent of cells that are polyploidal is not high, Dawson said. It’s only during late-stage cancer or after treatment that there is an observable amount of these cells.
Polyploidal cancer cells form through endoreplication, a defective form of mitosis, where the cell clumps up rather than separating normally, Dawson said. They also form through “cell fusion,” where smaller normal cancer cells group together. Cell fusion increases substanitally when cancer is treated with high-dose Taxol, she added.
Literature shows that these giant polyploidal cells survive after treatment, which increases production of non-polyploidal cells that can “restart” the tumor, Xuan said.
Even though the focus has been on breast and ovarian cancer, polyploidal cancer types do not seem limited to specific cancers, Dawson said, adding that more research is needed.
The difference between normal and giant cancer cells can be better understood through the tortoise and the hare analogy, Dawson said. “(The smaller normal cancer cells) can move around pretty fast, but they cannot move directionally,” she said, while the giant cells have direct paths and can transport more cancer overall.
Since there are multiple subtypes of cancer cells, including polyploidal cells, it is very difficult to treat an entire cancer population, Xuan said.
By studying these giant cancer cells and their function, researchers can improve treatments and have better diagnostics than those used in the past, said Benjamin Tang, assistant adjunct professor at the University of California at San Francisco.
“(We need to) isolate for these polyploidal cells, which would allow us to get a more in-depth understanding of the molecular composition of these cells,” Xuan said.
“It’s a very exciting study, as it explores aspects of specific cancer cells that we typically don’t look at,” Tang said.
There are a few companies looking into using drug-loaded nanoparticles for cancer treatment, but more research is needed, Tang said.