Almost immediately after taking office, former President Donald Trump issued Executive Order 13769, “Protecting the Nation from Foreign Terrorist Entry into the United States,” banning travel and immigration from seven predominantly Muslim countries, including Iraq, Syria, Iran, Libya, Somalia, Sudan and Yemen. Using patient data from Minneapolis-St. Paul, Minnesota, University researchers found that Muslim Americans experienced several changes in their health care use in the aftermath of what was eventually referred to as the 2017 “Muslim ban.”
The data showed a rise in missed appointments and emergency department visits, according to a 2021 study published in the Journal of the American Medical Association.
“Islamophobia and restrictive entry policies have been associated with worse health outcomes among migrants,” according to the study. These policies have led to increased “discrimination, hostility and ‘othering’” toward Muslim Americans, resulting in “an increase in hate crimes and social hostility” toward the Muslim population over the past two decades, the authors of the study wrote.
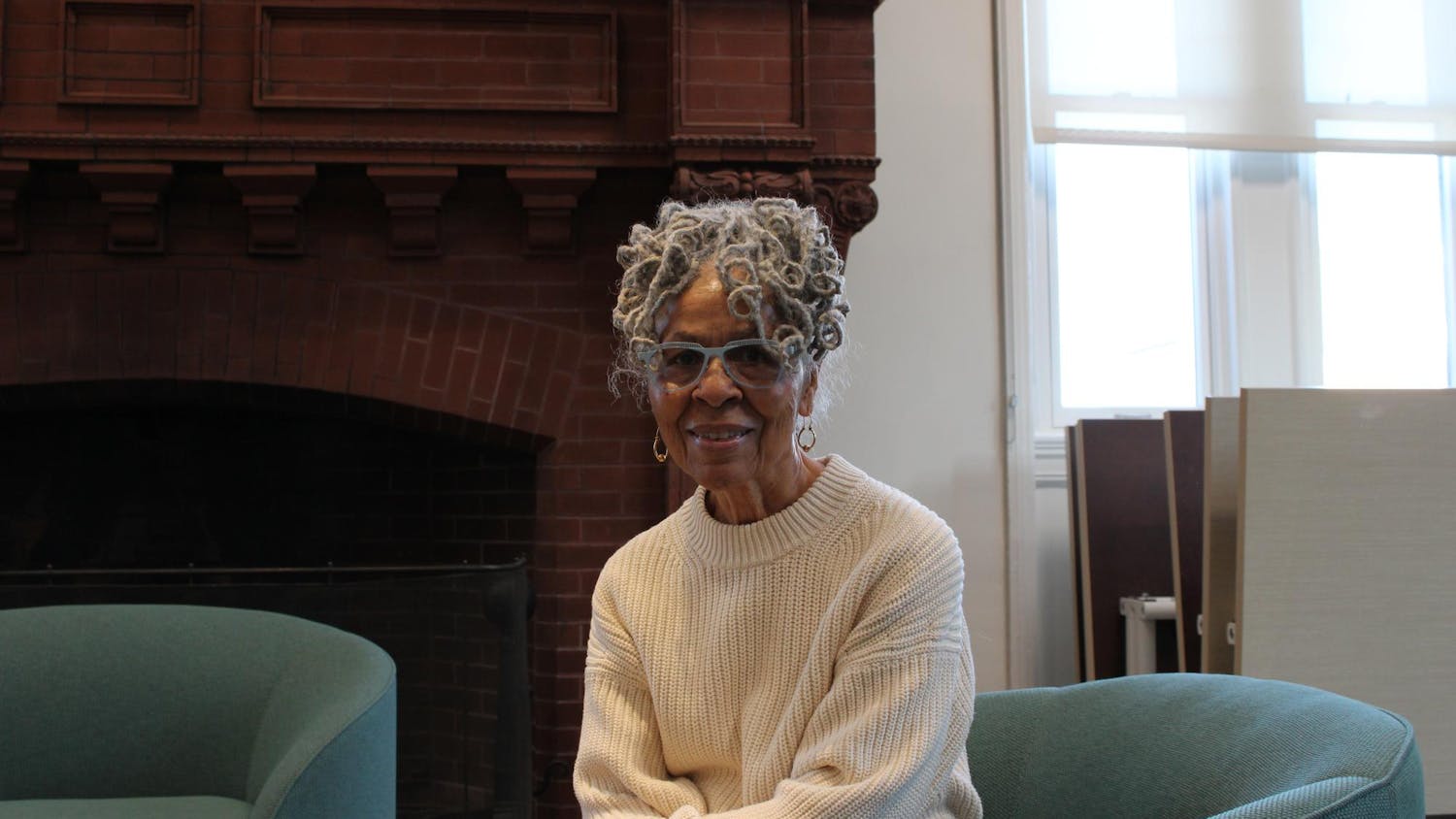
“We wanted to look at the health effects of the immigration policies of the Trump administration using quantitative methods,” said lead author of the study and assistant professor of emergency medicine Elizabeth Samuels.
In order to examine the impacts of the “Muslim ban” executive order on health care use trends of Muslim Americans, the researchers used Minneapolis-St. Paul patient data collected by insurance company HealthPartners. Unlike many insurance companies, HealthPartners collects data on patients’ country of origin, allowing the researchers to identify immigrants from predominantly Muslim countries — both those included and not included in the ban, according to Samuels.
“We chose Minneapolis because they have a very large Somali community and population, and … most folks who come here from Somalia are Muslim,” Samuels said.
The researchers analyzed health care utilization trends in primary care and emergency department use in the Muslim population living in Minneapolis-St. Paul before and after passage of the executive order. The study also analyzed the number of visits for stress-responsive diagnoses for conditions such as incidents of heart attacks, suicidal ideation and assaults.
“Immediately following passage of the ban, we saw an increase in (emergency department) visits overall and (emergency department) visits for stress-responsive diagnoses,” Samuels said. Within the population being studied, there were an additional 232 emergency department visits in the year following the passage of the ban than the researchers had predicted using the available patient data from previous years. The researchers also found that, relative to the prediction, patients missed an additional 101 primary care appointments.
Missing medical appointments can exacerbate future health issues, said Aasim Padela, a study author and professor of emergency medicine, bioethics and the medical humanities at the Medical College of Wisconsin.
These results “reflect elevated cumulative stress due to multiple restrictive policies and an increasingly hostile climate toward Muslim immigrants and refugees in the U.S.,” the authors of the study wrote.
The findings demonstrated “a level of psychological distress that was pervasive in the community for Muslims from Muslim majority nations that were mentioned in the Muslim ban,” Padela said.
“I’m not surprised that this stress would manifest in missed doctors’ appointments,” said Assistant Professor of Education Andrea Flores, who was not involved in the study but has conducted ethnographic research on the educational experiences of Latinx youth immigrants.
The study authors hope their findings influence further research into the impact of foreign policy on health inequities faced by minority groups in the U.S. But one challenge of collecting data about religious identity is that patients might not want to disclose that information for fear of discrimination, Samuels said.
Muslims “have experienced a lot of discrimination and xenophobia and racism,” Samuels said. “Understandably, there’s a lot of skepticism and lack of trust.”
Samuels noted the importance of identifying the people “for whom you’re trying to mitigate health inequities,” but added that researchers should “be careful not to stigmatize or cause undue surveillance or other problems in the community.”
This study “shows the importance of policy’s impact on people’s actual lives, including their health,” Flores said. “Policies have unintended consequences, and those consequences are human ones that directly affect the lived experience of many people.”
The study prompts people to “think about the link between foreign policy-related decisions and the health of communities in the United States. If someone makes a decision about whom to bring into the country … it impacts individuals in our own community and our own country who are from those nations and how they interact with the healthcare system,” Padela said. “Foreign policy is also health policy.”