Ethnic minorities are less likely to receive adequate treatment for anxiety disorders than non-minorities, according to the results of a new study from University researchers.
The researchers evaluated a number of different factors, such as the income and education level of patients receiving treatment for anxiety, concluding that minority patients received worse anxiety treatment than non-minority patients even after controlling for other related variables.
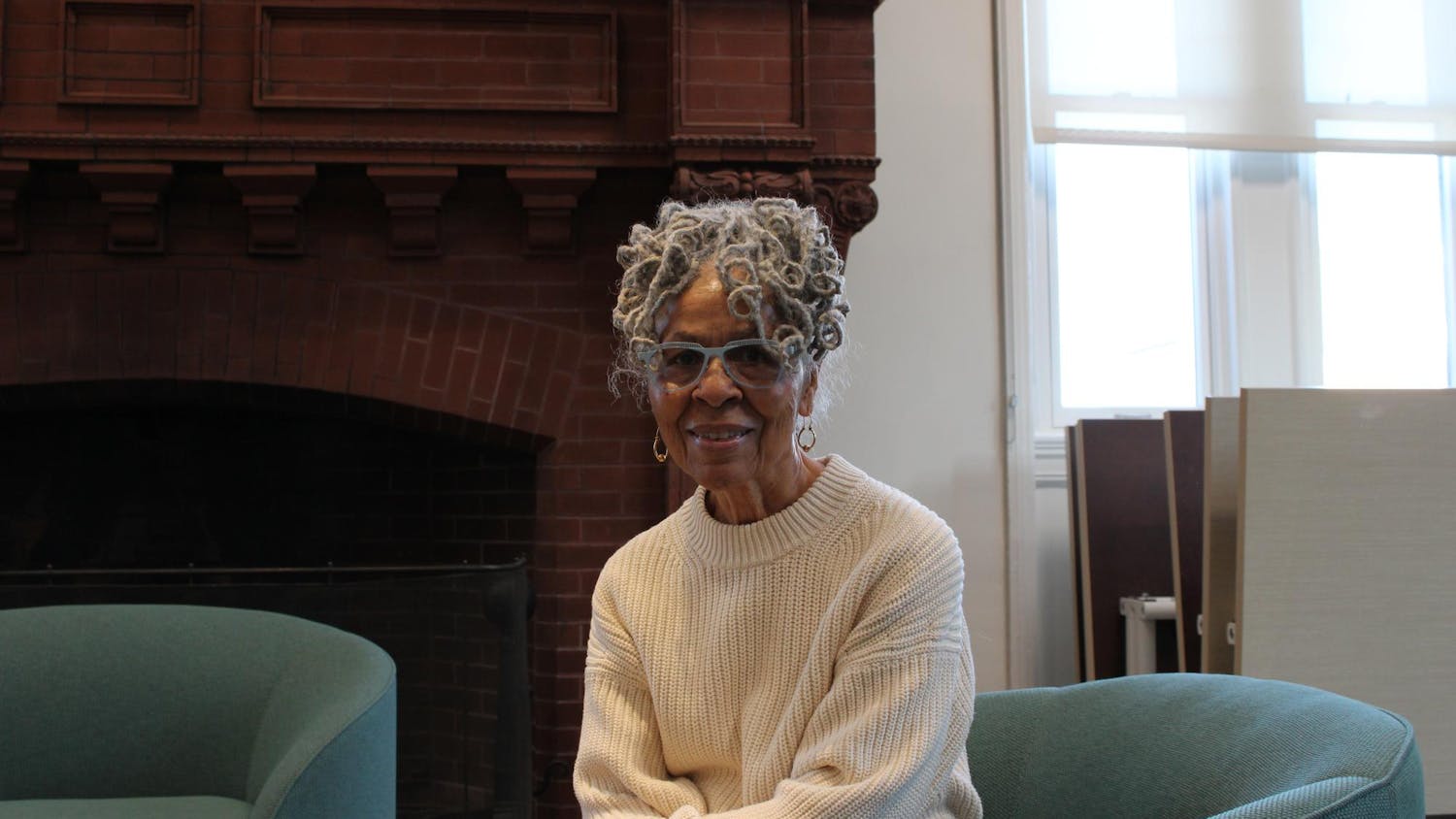
“Minority status was a unique factor. It wasn’t about income. It wasn’t about educational level. It wasn’t insurance,” said Risa Weisberg, associate professor of psychiatry and human behavior, and one of the study’s lead authors.
In fact, patients in the lower income brackets actually got better treatment for their anxiety, she added.
“Being a minority member made you less likely to get good therapy, but being in low income made you more likely to get good therapy,” Weisberg said.
The disparity in adequate treatment along ethno-racial lines is a phenomenon “I would think healthcare policymakers would want to attend to without delay,” wrote Boston University Professor of Psychology and Psychiatry David Barlow, who was not involved with the study, in an email to The Herald.
As to why minorities were less likely to receive adequate treatment, “Community attitude is part of it, trust of the system is part of it,” said Ethan Moitra, assistant professor of psychiatry and human behavior at the Alpert Medical School and one of the paper’s co-authors.
Research has also shown that mental health providers often approach decision-making differently depending on the patient’s background, headded.
Over the course of the study, the researchers observed an increase in the overall number of patients receiving adequate treatment for anxiety.
But this increase is deceiving, Weisberg said, adding that it does not reflect a true rise in the level of adequate treatment but is instead due to a large number of patients trying treatment for a short period of time.
Defining adequate treatment was a major challenge in the research, due to the lack of material available on these standards.
“For the most part, people in the field really haven’t taken the time to define these treatments,” Moitra said. “Ultimately, the priority for treatments may vary depending on the individual and the severity of their needs.”
The study based treatment adequacy on two factors — medication and therapy.
Patients had to be taking a medication known to be effective for an anxiety disorder, Weisberg said. This drug had to be taken “at a dose that experts in the field would consider adequate” and “consecutively for at least eight weeks.”
In addition to medication, the quality of patients’ therapy sessions was also taken into account. “Just because somebody’s doing some sort of behavioral or cognitive technique doesn’t necessarily mean it’s going to be quality treatment,” Moitra said. “We really got very specific as to what was going on inside of these treatment sessions,” he added.
“The good news of the study is that most patients eventually received potentially adequate treatment for their disorders,” wrote Boston University Professor of Psychology Stefan Hofmann, who was not involved in the study, in an email to The Herald.
“The bad news is that cognitive behavioral therapy, the most cost-effective treatment — especially in the long term — was rarely provided,” Hofmann wrote. Cognitive behavioral therapy employs talk therapy sessions, rather than drug regimens, to address behavior and mood disorders like anxiety.
The study was a “naturalistic, observational study where we collected information about patients’ anxiety symptoms, treatment and functioning, without us intervening on any of those factors,” Weisberg said. Unlike many other observational studies performed in a medical context, this study looks “at people longitudinally, and that’s rarely been done in these naturalistic treatment studies before,” she added.
Because the study’s results come from “a sample of convenience” — with respondants surveyed exclusively in New England and in a self-selecting manner — it is unclear if these results could be generalized to the entire population of primary care patients, Weisberg added.
“Clearly, disseminating adequate care, especially cognitive behavioral therapy, should be one of the most important priorities of any initiative to improve access to mental health care,” Hofmann wrote. “This not only reduces the suffering of millions of Americans but also saves the tax payers an enormous amount of money through the reduction of indirect cost.”
ADVERTISEMENT